Periodically in this blog, lately once a year, I review all of my professional accomplishments, including honors, talks given, papers published, and more for the past year. Last year was a transitional year for me professionally, as I stepped down from two leadership positions as Chair of the Oregon Health & Science University (OHSU) Department of Medical Informatics & Clinical Epidemiology (DMICE) and from being Director of the OHSU Biomedical Informatics Graduate Program. As seen in this post, however, my productivity did not miss a beat in 2023, and in fact I am enjoying my work as much as ever by being able to focus on teaching, research, and writing.
I was awarded one honor in 2023 which was the Lifetime Achievement Award from the HIMSS Oregon Chapter.
I also gave a large number of invited talks, some in person and others virtual. Links to my slides and references, and for some, videos of the talks, are available on my Web site. The talks given include:
- From the Longwood Medical Area to Oregon: An Informatics Career Journey - Harvard Clinical Informatics Lecture Series (virtual), January 24, 2023
- Introduction to Informatics: What You Should Know as a Health Services Researcher - VA Health Services Research & Development Advanced Fellowship Program (virtual), March 7, 2023
- Translational Artificial Intelligence (AI): The Need to Translate from Basic Science to Clinical Value - University of Iowa Distinguished Biomedical Scholars Lecture Series, Iowa City, IA, March 9, 2023
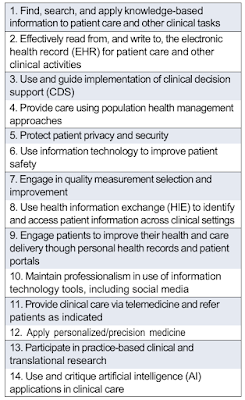
- Competencies and Curricula Across the Spectrum of Learners for Biomedical and Health Informatics - University of Texas Southwestern Clinical Informatics Research Colloquium (virtual), May 18, 2023
- Informatics Innovation: Quarter-Century of OHSU Leadership - HIMSS Oregon Chapter Annual Conference 2023, Portland, OR, June 1, 2023
- Biomedical and Health Informatics: An Essential Discipline for 21st Century Medicine - Informatics Colloquium, Department of Pathology, Indiana University School of Medicine (virtual), July 19, 2023
- Biomedical and Health Informatics: An Essential Discipline for 21st Century Medicine - Department of Medicine Meet the Global Expert Webinar, University of Cape Town, South Africa (virtual), August 17, 2023
- Artificial Intelligence: Implications for Health Professions Education - Keynote Talk, Commission on Accreditation for Health Informatics and Information Management (CAHIIM) Summit on Higher Education (virtual), September 28, 2023
- Artificial Intelligence in Medicine: Promise and Peril - Grand Rounds, Department of Pathology and Laboratory Medicine, OHSU (virtual), October 4, 2023
- ChatGPT and Other AI Tools for Medicine and Medical Education - International Association of Medical Science Educators (IAMSE) Fall 2023 Webcast Seminar Series: Brains, Bots, and Beyond: Exploring AI's Impact on Medical Education (virtual), October 5, 2023
- Artificial Intelligence: Implications for Health Professions Education - Educator’s Collaborative, OHSU (virtual), October 18, 2023
- Artificial Intelligence in Medicine: Promise and Peril - 33rd Infectious Diseases Society of Oregon Annual Meeting, Salem, OR, October 26, 2023
- Artificial Intelligence in Medicine: Promise and Peril - Public Health Officers Caucus of Oregon (virtual), November 28, 2023
- Artificial Intelligence: Implications for Informatics Education - OHSU DMICE Conference, Portland, OR, December 14, 2023
I also participated in a number of panels at meetings:
- Current Clinical Evidence and Available Technology - Voice AI Symposium, Bridge2AI-Voice Consortium, Washington, DC, April 19, 2023 (Panelist)
- Program Sustainability - Office of the National Coordinator for Health Information Technology (ONC) Public Health Informatics & Technology (PHIT) Workforce Program (virtual) June 20, 2023 (Panelist)
- Strategies for Effective and Equitable Partnerships - Third Meeting of the Data Science Initiative for Africa Consortium, Kigali, Rwanda, November 8, 2023 (Panelist)
- Building Human and Data Capacity in the NIH Data Science for Africa Initiative - AMIA Annual Symposium 2023, New Orleans, LA, November 13, 2023 (Panelist and Moderator)
- Bridging Training Gaps through Voice: An Ethics-based Approach to Teaching Trustworthy AI - AMIA Annual Symposium 2023, New Orleans, LA, November 14, 2023 (Panelist)
- Generative Applications of Large Language Models for Medical Education and Knowledge Searching: Shall We Count on ChatGPT and Co.? - AMIA Annual Symposium 2023, New Orleans, LA, November 15, 2023 (Panelist)
I appeared on an episode of the Health and Explainable AI Podcast from the University of Pittsburgh HexAI Research Laboratory.
I was awarded one new grant in 2023 but continued to be busy with my four existing grant projects. The new grant was an administrative supplement to an existing grant, the Bridge2AI Voice as a Biomarker project, to develop a summer school for college undergraduates and students in clinical training. My existing grants include a National Library of Medicine (NLM) R01, NLM training grants for informatics predocs and postdocs and for a college summer internship program, another training grant in the Data Science Initiative for Africa, and being part of the Skills and Workforce Development Module of the Voice as a Biomarker project.
I continued my teaching in 2023. As always, a major part of my teaching my introductory course in biomedical and health informatics, which is offered as BMI 510/610 at OHSU, the AMIA-OHSU 10x10 ("ten by ten") course, and as MINF 705A/709B, a medical student elective at OHSU. I also gave my annual lecture to OHSU medical students in their first month of class, Information is Different Now That You're a Doctor, on August 25, 2023.